Abstract

Introduction
Diffuse large B cell lymphoma (DLBCL) that relapses or is refractory (R/R) to first-line treatment has poor prognosis. Patients fit enough for high-dose therapy and autologous haematopoietic stem cell transplant (autoHSCT) may achieve a prolonged second remission. However, there is no standard of care for patients who are not eligible for this potentially curative approach. Following the report of rituximab (R), gemcitabine (G), cyclophosphamide (C), vincristine (V/O), prednisolone (P) (RGCVP) as frontline management of less fit patients with DLBCL (Fields JCO 2013), we sought to establish the efficacy of RGCVP as second-line treatment in patients previously treated for R/R DLBCL who are not candidates for intensive management.
Methods
A retrospective study of patients presenting with R/R DLBCL from 01/01/2010 to 31/12/2016 was undertaken across three hospitals in London, United Kingdom. Patients who were a) over the age of 18 years, b) determined not fit for high-dose therapy by their primary treating physician and c) managed with RGCVP as second or subsequent line treatment were included and their demographics, disease characteristics, management and clinical outcomes are presented here.
Results
Over a median follow-up of 30 months, 24 patients were identified who met the inclusion criteria: 18 as R/R de novo (dn) DLBCL and 6 as R/R transformation to DLBCL following indolent non-Hodgkin lymphoma (iNHL; 5/6) or Hodgkin lymphoma (HL; 1/6). Median age was 77 years (range 40 to 85; IQR 71 to 79) with a gender ratio of 1F:1.4M. Median ECOG PS was 2 (range 0-3) and the majority (n=15) had at least one significant co-morbidity. Most (n=19; 79%) had 1 prior line of treatment (median 1; range 1 to 3) for DLBCL. All had previous rituximab while 23/24 (96%) had received anthracycline (doxorubicin; H) as RCHOP/RminiCHOP and 1 had RCVP as prior treatment for DLBCL. Only 1 patient had prior autoHSCT. Of the transformed cases, 4/6 had treatment of preceding lymphoma: chemotherapy for iNHL (n=2) or radiotherapy for iNHL and HL (both n=1). Ahead of RGCVP, median stage of R/R DLBCL was 4 (range 1 to 4).
In this frail population, treatment toxicity was a particularly important consideration and upfront elective dose reductions were made in almost half (11/24; 46%). Patients completed a median of 4 cycles RGCVP (range 1 to 6) with 72% of the cohort completing their planned course. Haematological toxicity was common (grade 3/4 neutropenia (11/15; 73%), thrombocytopenia (9/16; 56%) and anaemia (6/16; 23%)) but well tolerated. Primary GCSF prophylaxis was used for these elderly, pre-treated patients and while infection was the most common non-haematological toxicity, occurring in 2/3 of patients, there were no infection related deaths. Main reasons for early RGCVP discontinuation were disease progression (n=3) or treatment related toxicity (n=2). While the majority of patients (71%) had at least 1 hospital admission (median 1, range 0 to 3) during their RGCVP course, mostly associated with infection, no deaths were attributable to treatment related toxicity.
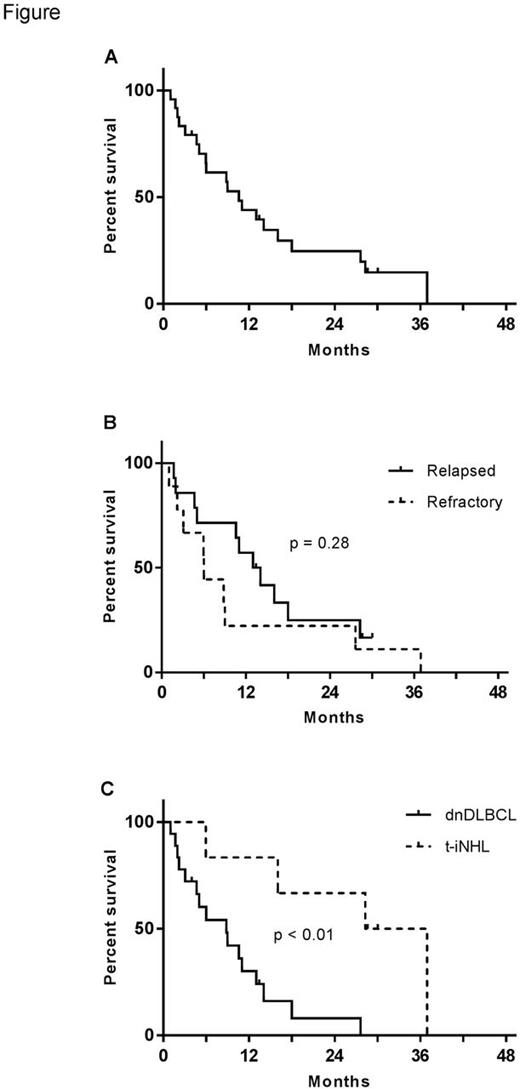
Most patients (20/24; 83%) had responsive disease, including 10 (42%) complete (CR) and 10 (42%) partial remissions, with the remainder stable (n=1) or progressing (n=3). Median overall survival (Figure A) and progression free survival were 11 and 8 months, respectively. There was a trend (p=ns; Figure B) to shorter survival in patients who were refractory to previous line therapy compared to those who relapsed. R/R transformation may have a better outcome with this approach as median survival was 33 months (compared to 9 for R/R dnDLBCL; log rank p < 0.01; Figure C). Subsequent management included local RT, oral chemotherapy, novel agent clinical trial, pixantrone or no further treatment. At the time of analysis, 83% (20/24) patients had died with only 2 deaths not attributable to lymphoma (cardiac events in patients maintaining CR after RGCVP at 18 and 37 months).
Conclusions
In this pilot study, of older, frail patients with DLBCL that is resistant to RCHOP, the RGCVP regimen as second-line therapy can be delivered safely and with promising activity in a population with particularly poor prognosis who continue to be managed with palliative intent. These results provide a platform for future prospective studies to validate this novel approach for R/R DLBCL arising as de novo or transformed lymphoma.
Stanley: Roche: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Janssen: Honoraria, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau. Fields: ADC Therapeutics: Research Funding; Takeda, Roche, MSD: Consultancy, Honoraria. Wrench: Roche: Honoraria, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal